Oh My Fungus!
A reader took off her pedicure and got a nasty surprise. This blog is about Toenail Fungus.
I was recently asked by my lovely subscriber, Sandy, about a toenail issue she noticed after removing old polish from a pedicure. Sandy is in her early 50’s, a health professional, and was about to go on a cruise and wanted her nails to look nice. This was certainly an unwelcome surprise when she took off the old polish!
Sandy’s most pressing questions regarded her cruise. Should she paint the nails over this damage? No, for reasons I will explain below. Should she avoid the pools? Not necessarily, but she was right about fungus liking water. In fact, fungus likes three conditions to grow: 1. Moisture, 2. Heat, and 3. the Dark. As I like to tell my patients, if you leave a wet towel in a warm, dark place—it’s going to grow fungus. Think about times you have forgotten to take your wet laundry out of the washing machine. You can almost smell it now, can’t you? It’s the perfect example of a warm, wet, dark place setting up fungus and molds to grow.
The first thing that strikes me about Sandy’s fungus issue is that much of this whiteness and damage looks superficial (on the surface). She should be able to remove most of it with a file or with the help of her podiatrist. Sandy could try to remove some of the discoloration at home with nail files like the ones pictured here:
She could start with the course side of either type of file to remove the whiteness, then use the finer side to try to restore her nail to its normal smooth sheen. The problem with these tools is that a flat file or bulky file would likely not be able to follow the curve of Sandy’s nail without harming her skin as well. She also may not be able to reach superficial nail damage in the corners of her nail where they curve inward.
What a Podiatrist Does for Thick Nail Pain Relief:
A podiatrist can use a mechanical tool with a sanding bit on the end to remove superficial nail damage (see below). If the damage is completely sanded off by your podiatrist, you may not need an oral (by mouth) nail fungus treatment or even a topical one. If it doesn’t sand off, an oral medication is your next choice. However, nail fungus is considered a cosmetic issue, so IF IT DOESN’T HURT, medication is not necessary. If there are no pain or ingrown toenail infections associated with your fungus, then medication is a COSMETIC choice. Toenail fungus doesn’t spread from your nails to your feet or from nail to nail. It needs the warm, moist, dark environment to spread—not contact.
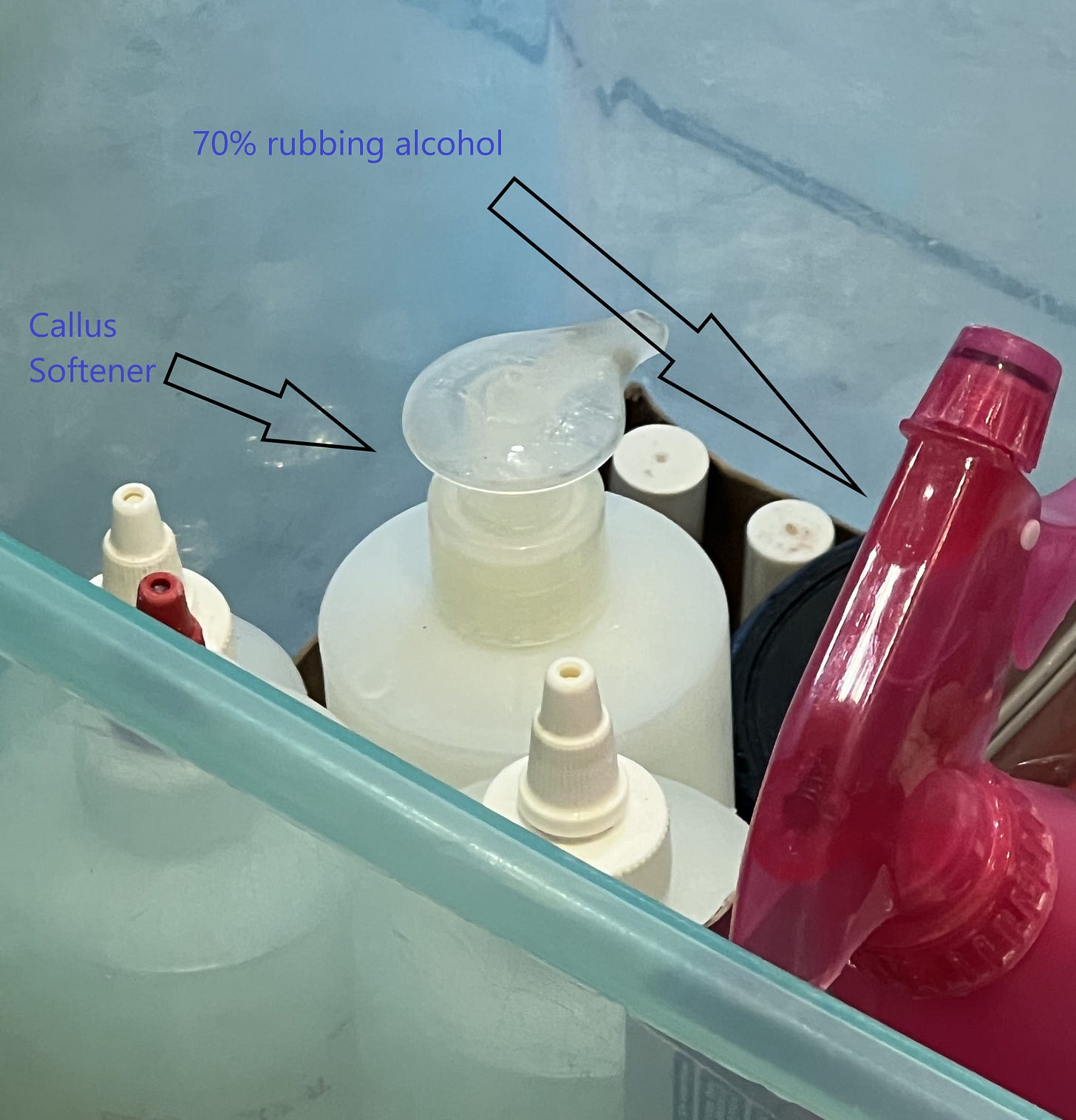
My first choice of treatment is sanding the damaged nail surface to relieve pain and assess if the damage goes all the way through the nail. If it does not, give yourself a few months or so to attempt to grow the damaged area of the nail out completely. Nails grow about 1 mm per month so you can actually track if it is moving on out. I advise my patients not to have a pedicure over damaged nail. Sandy’s concern about the pool is real—if she spent a LOT of time in a pool—to the point of pruning her skin, it is possible her nail damage could worsen as it would be harder for her damaged nail to get and stay dry when she gets out of the water. In her case, I would consider shorter dips in the pool, and advise her to towel her toes off thoroughly after swimming or bathing. To ensure the nails get completely dry, I recommend using hand sanitizer, or 70% rubbing alcohol to dry the cracks in the nails and under loose areas of nails. Hand sanitizer is largely made from isopropyl alcohol so a quick dab could be really efficient and easy for her to acquire to help prevent further nail damage on her cruise.
How Did I Catch the Fungus?
In general, you don’t CATCH fungus on your toenails. It develops when the conditions are right for it to grow (Hot, Wet, Dark). Usually there is some trauma which damages the top or underside of the nail creating looseness or pitting/scratches.
Your last pedicure can be the source of trauma if a harsh gel or shellac was used, or if your pedicurist scraped the surface of your nail to remove it.
An ingrown toenail that drains for a long time can also cause increased moisture exposure that can cause fungus. I have seen people get fungus after having ingrown toenail procedures by wearing non-stick pads or bandages over the procedure site, trapping moisture over a draining nail. I recommend dry gauze and antibiotic ointment after nail procedures instead of non-stick dressings for that reason.
You may have developed conditions for fungus by working in the hot sun wearing sweaty socks in boots. Work boots tend to seal sweat in your shoes and promote fungus.
Shoes that pinch or are too short (especially if you have a long 2nd toe) can set up certain toenails for damage.
If you have a curved toe (hammer toe) which nail hits the ground when you walk—fungal like damage can occur.
Feet slamming into the ends of your shoes due to distance running or improperly fastened footwear can set up trauma causing fungus.
You could drop something on a toenail, setting up a blood blister under the nail, which lifts the toenail and creates a space for moisture to collect.
Any of these events are common causes of toenail fungus. Controlling whether your nails are in a wet, hot, and dark environment will help you control whether you get fungus, or whether it returns after treatment.
Do I Need Oral Treatment?
If your lifestyle prevents you from having a healthy foot environment, don’t bother with oral medications—just debride nails as often as needed for symptom relief. Fungus will recur if you work and live in a climate where your feet get wet and stay wet. I don’t even bother with medication for my patients who are chicken farmers and work in the heat in rubber boots. God bless—you need to be retired first. Your feet are going to have fungus. Same with my brave roadside construction workers—unless you can change wet socks to dry frequently—fungus is likely going to enjoy your feet and toes. If you can’t control the wet, hot, dark environment around your toes, you need to debride as needed for pain and consider waiting to medicate until you CAN control the environment around your toes.
A Word on Moldy Smelling Shoes
If your shoes smell like mold, they are telling you they are great incubators for your fungus conditions. Please set them, and any insoles in direct sunlight until they don’t stink (usually a few hours). You may wash them first if they are washable, adding vinegar to the wash load, and being careful to dry them ALL THE WAY in the sun before wearing. Do as often as needed. Mesh top covers—shoes with little holes in the fabric that let you feel the wind when you swing your leg—are the way to go if you suffer from fungus of the nails or feet. Light-colored shoes are better for preventing fungus than dark. If you wear dark shoes and dark socks with no breathing room for your feet or toes—you are making your fungus fight harder to win. Just facts. Here is an example of a light colored shoe with mesh topcover
Damage from Pedicure Salons:
In my opinion, people who have nail damage from pedicure salons usually get it by layering polish or gel over nails that have some superficial damage. When you soak your feet in the salon, that damage traps moisture which can stay under the polish or gel for the many weeks or months that you leave the polish on. It is common with gel or shellac that the nail can look white and scratched when it is removed. Or your pedicurist could try to speed up the removal of your gel by scraping it off. This is enough damage to POTENTIALLY set up fungus. Do I get pedicures? Yes. The leg massage, the hot towels, the massaging chair, and someone who can paint my nails and it not look like a kindergartener did it? What can I say. I love them. For my medical situation, it’s worth the risk. The hot towel:
However, I inspect my nails before I let them apply polish. I recommend that if you see superficial nail damage after getting a pedicure, and your pedicurist can NOT sand or polish it off, that you WAIT for this damaged nail to grow out before painting your nails again. I believe this painting over trapped moisture to be the most common cause of damage/fungus from pedicures. A good salon will also use the following:
Sterile instruments—either heat sealed in a bag or soaking in a cold sterilization solution:
A fresh, sterile sanding bit:
YOUR OWN FILES which haven’t been used by other clients (which they should offer to sell you on your first visit):
A liner for the soaking bath, if soaking is used:
70% rubbing alcohol on your nails to remove moisture before painting/shellacking:
On Topical Antifungal Medication:
I am not impressed with the data on topical antifungal treatments. The only FDA approved topical medication for years (Ciclopirox/Penlac) only has a 6-7% effective rate and needs to be applied daily for at least ten months and removed weekly. In my opinion, it builds up horribly on the nails and looks awful. Think of it this way—its failure rate is 93-94%. I do not currently recommend any topical medications to CURE fungus. Tea Tree oil and Vicks do not cure nail fungus. Vicks may soften the nail— like 40% urea I describe below, and can be used for symptom relief (not a cure). But it doesn’t have the data of Urea 40, which I describe below.
What if it isn’t Fungus?
Medically, your podiatrist should ask you if you have psoriasis, as damage to the nail from psoriasis looks exactly like nail fungus. Oral medications typically won’t help you if you have psoriasis. If you have a yeast and not a fungus, you will need your doctor’s recommendation on medication as the most common antifungal medication, terbinafine, likely won’t help. See your podiatrist for further guidance.
What if my Nails are Painful?
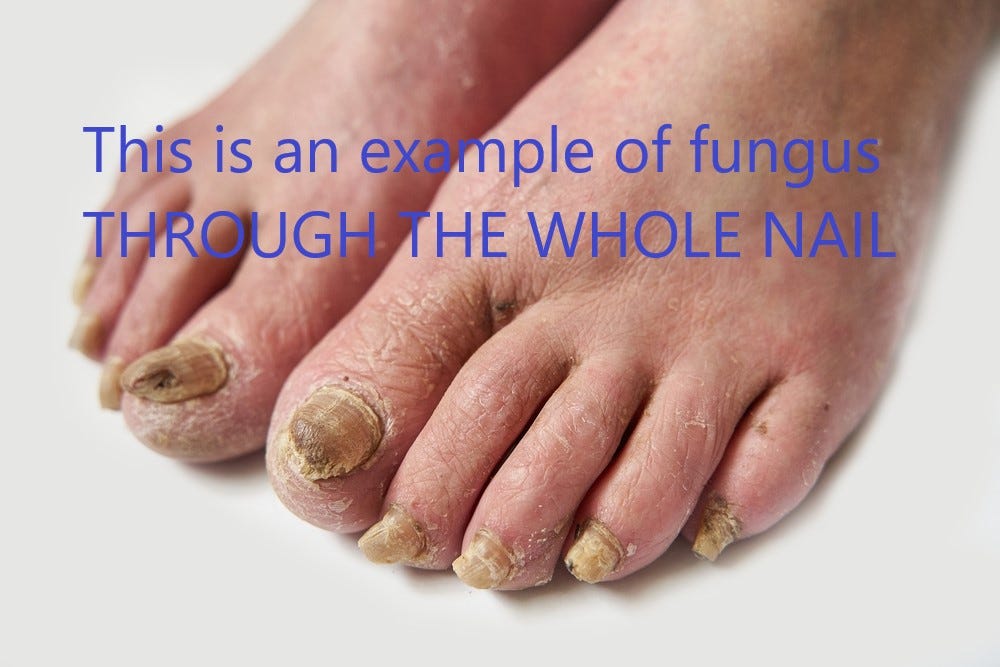
If your toenails are thick through and through, they can really hurt.
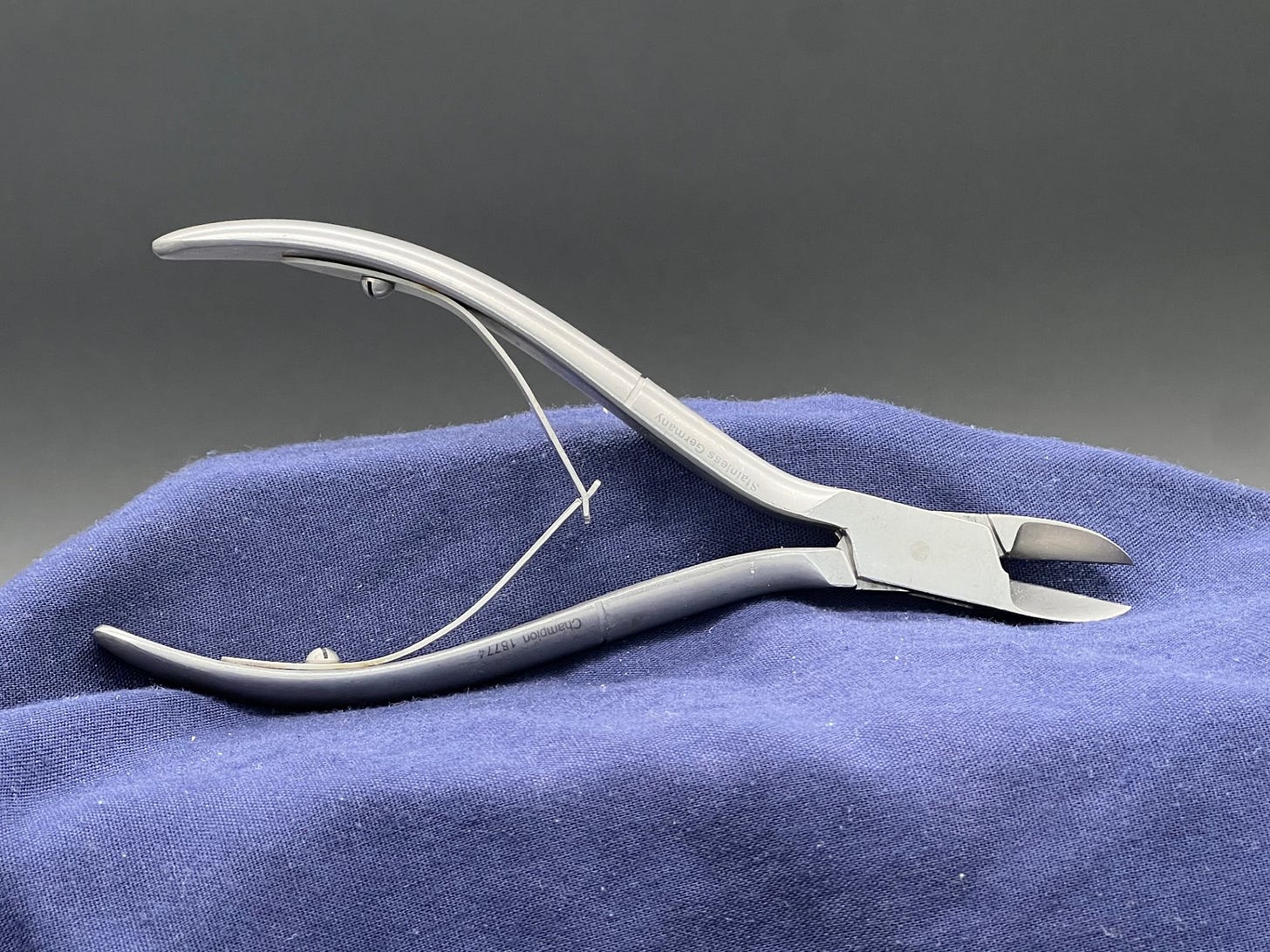
They can also get loose and fall off, which can be quite alarming. If your toenails cause pain, see your podiatrist for something called debridement (pronounced dee-Bride-Mint, or Duh-BREED-mint). Your podiatrist will use tools like these:
and usually these:
I like the coarse carbide bits because they work faster and have less risk of producing heat which my patients find painful.
Can I Debride My Own Nails at Home?
There is a research-proven effective debridement technique you can do at home. The standard for home debridement is to use a 40% urea cream or ointment (such as Urea 40 on Walmartdotcom). The following home treatment should be done at bedtime nightly until you see results:
Apply regular petroleum jelly to the skin surrounding the nail as a buffer.
Apply the 40% urea cream or ointment to the nail itself.
Occlude the nail (this typically means covering the nail with a light layer of plastic wrap or an adhesive bandage like a Bandaid) and keep it in place overnight by wearing a sock or perhaps securing with medical grade tape. Please be careful not to strangle your toe and perform your own amputation. That kind of thing is best left to ranchers gelding sheep or cattle. So, nothing tight around the toes please.
Sleep with your dressing on and remove it in the morning. Wash the foot with soap and water and hopefully find the nail beginning to easily flake off in layers with your own home nail cutting equipment.
Do this nightly until you can debride your nails down to a manageable shape or height. If this doesn’t relieve your pain, or this process doesn’t appeal, or you have serious underlying health conditions such as diabetes or poor circulation, please see your podiatrist and avoid self-care.
What Medication Will My Podiatrist Give Me and IS IT SAFE?
The most common medication your podiatrist will prescribe for nail fungus is called terbinafine (Lamisil). Oral antifungals do not affect the existing nail damage but help the new nails to grow out healthy, pushing out the diseased nail. It takes toenails about 1 mm per month to grow, and the big toe can take anywhere from 9 months to a year or more to grow out. You should notice a horizontal line of healthy nail pushing out the sick nail toward the end of your toe. You should keep clipping off the sick nail as it grows out until it is gone. This picture shows what that may look like:
Terbinafine used to be very expensive but is now generic and cost effective—sometimes as low as $10/month. This medicine has been known to harm the liver and can’t be taken with certain medications. I recommend always filling your prescriptions at the same pharmacy so your pharmacist can check for possible medication interactions before filling this and any other medication. The last data I read suggested terbinafine has about a 70% effective rate clearing up toenail fungus infection. If your doctor prescribes it for 90 days, they will check your liver first, and sometimes mid prescription course (at 6 weeks) to make sure the medication isn’t harming your liver. I never prescribe terbinafine if your liver enzymes were significantly elevated, or if you are on a medication that interacts with it (such as coumadin and some cholesterol medications). In my practice, I follow research-based guidelines that indicate that a one-month daily dose of terbinafine, followed by a one-month holiday from the medication, followed by another month of daily terbinafine is as effective as a three-month dose and doesn’t require additional liver testing at 6 weeks. Typically, all diseased nail will grow out within 12 months. If the diseased nail is making progress growing out, but has not fully grown out at 12 months, I repeat the one month on/one month off/one month on regimen. If it doesn’t work by 12 months, ask your podiatrist for alternative oral medications.
Disclaimer:
This information represents MY experience with terbinafine (and nail fungus) and NOT all data. As always, this information is designed to SUPPLEMENT your podiatry visit and not to replace it. I am not your doctor. Please seek medical advice from a podiatrist that knows YOUR medical history, especially if you have diabetes. Stay curious, and thank you for learning more about toenail fungus.